Have any questions? Feel free to contact us:
MACRA & MIPS
EHR Software
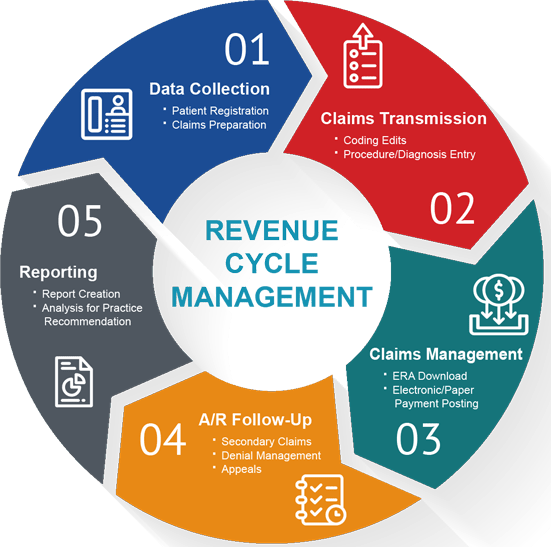
GreenSense Billing Quality Payment Program for your Revenue Cycle Management
In-depth knowledge about MACRA for your practice.
Hundreds of thousands of independent doctors and physicians have been able to incorporate the EHR into their practices, thanks to their commitment and dedication towards their patients. Since then, much has been changed due to the advancement of digital applications and innovation. The main objective of MACRA is to improve the care and convenience of Medicare patients. MACRA changes the payment system from volume to value and results.
As software certified by ONC 2015 EHR, GreenSense Billing meets all MACRA requirements. MACRA (Medicare Access and CHIP Reauthorization Act of 2015) introduces a new value-based reimbursement system, known as the Quality Payment Program (QPP), with includes three major and important changes in Medicare payments.
MIPS / APMs
Creating a new framework to reward doctors and physicians who provide better care. The two components of the QPP are:
--Merit Incentive Payment System (MIPS)
--Alternative Payment Models (APM)
Consolidates
Parts of three previous individual reports are grouped into a single system:
--Quality notification system for doctors (PQRS)
--Value based payment modifier (VBPM)
--Significant use of Medicare (MU)
SGR
Cancellation of the Medicare Sustainable Growth Rate (SGR) formula used to calculate doctors’ income reductions.
Medical snapshot of the patient
The patient chart shows and confirms data such as medications, allergies, problem lists, smoking and test results.
Apply Code Sets to annotate template fields
Quality measurements are calculated using ICD-10, CPT, LOINC and SNOMED codes
Patient Portal
Access your medical records 24 hours a day, 7 days a week.
Understanding MIPS in Detail for Your Ease
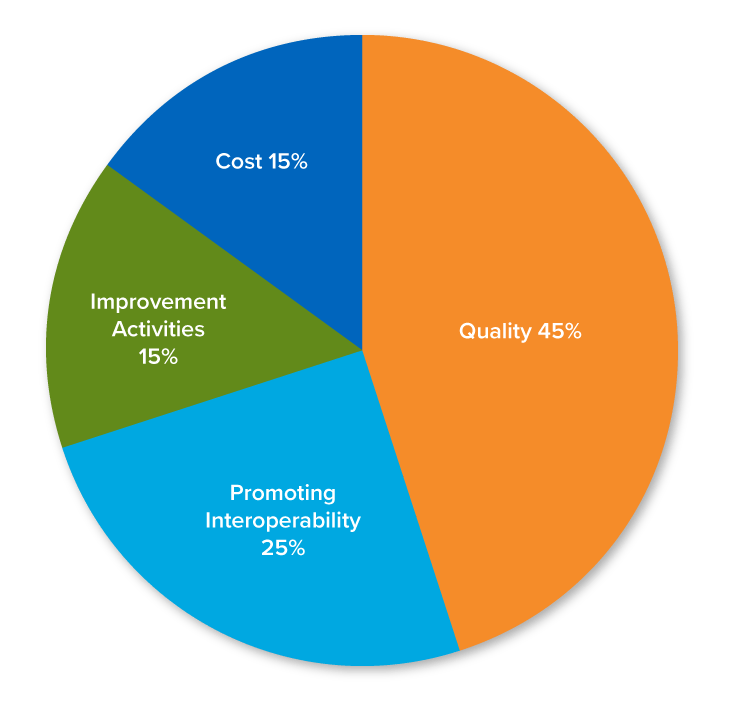
Discover the Weight of the 2019 Performance Category for MIPS
The Merit based Incentive Payment System (MIPS) is a program that measures the performance of an appropriate physician and compares it with that of their peers. MIPS is a budget based independent program. Medicare positive payment adjustments are funded by those who receive negative payment adjustments. Payment adjustments are made for Medicare Part B payments for professional services that occur two years after the execution period. The total MIPS score for 2019 (year 3 of MIPS) will be applied to Medicare payments in 2021.
Quality
45%, 12 months
6 Measures
Promoting Interoperability
PI (formerly ACI) – 25%
Attest to 6 required measures, and 2 optional bonus measures, for a minimum of 90 days
Improvement Activities
(aka from proposed rule CPIA) – 15%
Complete 1-4 improvement activities for a minimum of 90 days
Cost
15%, 12 months
Take a closer look at the MIP Category Wise Scoring Overview
The second way to participate in MACRA is the APM route, where eligible doctors register and become “qualified participants” with an advanced APM and earn 5% of the payment incentive. Advanced APMs companies focus on providing high quality and affordable care: they can focus on specific clinical conditions, treatment episodes or patient populations.
The CMS’s QPP website contains resources that help physicians decide to participate in an APM and list those approved by RRQ MACRA. Many existing ACOs are on the Medicare’s list of APMs. If you are interested in becoming a QP with an APM, we recommend:
Online research on certain approved extended APM requirements. QPP.CMS.GOV – APM Form (https://qpp.cms.gov/apms/overview)
CMS Innovation Center website (https://www.cms.gov/)
Joint savings program website (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about.html)
Verify that the APM you want to accept and question and meets the requirements.
Request an appropriate APM for your practice.
GreenSense Billing complies with EHR regulations with fewer problems for you
Having trouble getting acquainted with the new requirements of MACRA and MIPS?
You are not alone with Our MIPS consultants having the experience of guiding you through the MIPS and providing you with the tools to achieve a positive MIPS score.

Start generating more revenue from your collections and minimize your overhead costs.















