Medical insurance eligibility verification is important as it ensures that patients receive the care they need while preventing billing errors and unnecessary expenses.
In this blog, we will explore the importance of insurance eligibility verification, how it works, and the benefits it offers to both patients and healthcare providers.
But first, let’s understand what insurance eligibility verification is.
Medical Insurance Eligibility Verification
Medical insurance eligibility verification, also known as benefits verification or verification of benefits, is the process of confirming a patient’s coverage before providing them with healthcare services. It involves verifying medical insurance, policy details, and coverage status to see if the medical treatment will be covered by the insurance or if the patient needs to pay out-of-pocket.
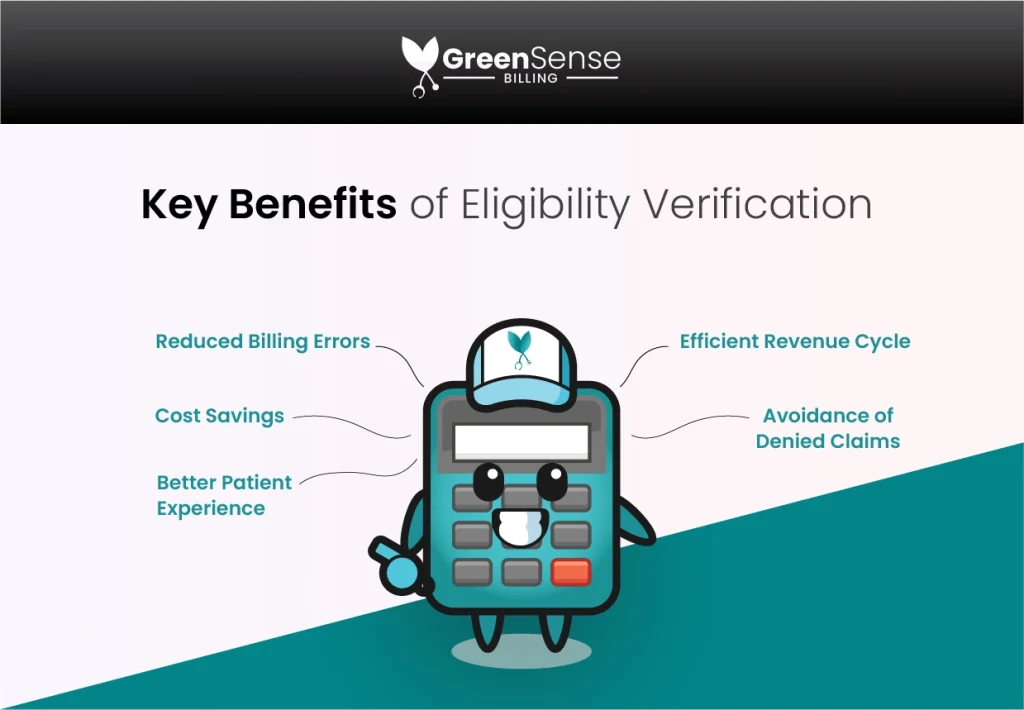
Key Benefits of Health Insurance Eligibility Verification
-
Reduced Billing Errors
Accurate insurance validation minimizes the chances of incorrect billing, preventing disputes and delays in reimbursement.
-
Cost Savings
Verifying insurance benefits beforehand helps patients avoid unexpected expenses by understanding their coverage limitations beforehand.
-
Better Patient Experience
Smooth insurance processing leads to improved patient satisfaction and loyalty as it confirms insurance coverage.
- Efficient Revenue Cycle
Proper patient verification streamlines the billing process, reducing administrative burdens for healthcare providers.
-
Avoidance of Denied Claims
Benefit verification in medical billing also reduces the risk of claim denials due to coverage issues.
How Medical Benefits Verification Works

Medical insurance eligibility verification involves several essential steps:
-
Gathering Patient Information
Healthcare providers collect patient data, including name, date of birth, insurance provider, policy number, and group number.
-
Contacting the Insurance Company
To verify health insurance Providers reach out to the patient’s insurance company & verify details like policy status, effective dates, and benefits.
-
Analyzing Coverage
The provider later assesses whether the insurance plan covers the requested service and identifies any limitations or exclusions.
-
Communicating with Patients
Next, patients are informed about their coverage status and any out-of-pocket expenses they may have to bear.
-
Updating Records
The verification of benefits information is then recorded in the patient’s electronic health record for future reference.
Importance of Benefits Verification for Patients
For patients, verifying eligibility coverage is important as it offers financial help and peace of mind. By knowing what services are covered and what expenses they may need to pay, patients can plan their healthcare budgets better.
Moreover, patient eligibility verification also prevents surprises in the form of hefty medical bills and allows patients to make informed decisions about their treatment options. Additionally, efficient insurance verification processes lead to shorter wait times and a more pleasant experience at healthcare facilities.
Importance of Benefits Verification for Providers
Every healthcare provider must check patient insurance eligibility to maintain a smooth revenue cycle and optimize operational efficiency. When they verify insurance coverage, they can avoid claim denials, reduce administrative overhead, and ensure timely payments.
Insurance verification in medical billing leads to improved cash flow and financial stability for medical practices. Furthermore, accurate healthcare verification helps build trust with patients, enhances the overall patient experience, and strengthens the provider-patient relationship.
Wrap Up
In conclusion, insurance eligibility and benefits verification is a fundamental aspect of the healthcare ecosystem. It benefits both patients and healthcare providers by ensuring financial security, reducing billing errors, and enhancing the overall patient experience. By embracing efficient verification insurance processes, medical practices can achieve better financial outcomes and provide top-notch care to their patients.
FAQs

1- What is eligibility insurance verification?
Eligibility insurance verification is the process of confirming if a patient’s insurance plan covers their medical services.
2- How to verify insurance benefits?
To verify insurance benefits, contact the insurance company and check the patient’s policy details and coverage.
3- Who can verify benefits for my patients?
Your front desk staff or medical billing service provider can confirm insurance coverage for your patients.



















